FT Health: Coronavirus — a time for trade-offs

Roula Khalaf, Editor of the FT, selects her favourite stories in this weekly newsletter.
Welcome back to the FT Health newsletter, which is relaunching as a monthly guide to the big issues at the intersection of global health and finance. Technology and investment are changing the face of healthcare while coronavirus is bringing an unprecedented focus on world health systems. This newsletter will provide news, interviews, data and the best health journalism from across the web.
FT subscribers sign up here
Non-FT subscribers register here
While much remains unclear about the precise characteristics of coronavirus, there is little doubt about the tragic human impact or the significant economic consequences But it also raises the need for trade-offs that require much greater reflection.
It is easy to attack the World Health Organization for not swiftly announcing an international health emergency or a pandemic at a time when much remains unclear; yet many companies and governments are imposing restrictions unilaterally that go well beyond what the best evidence would suggest is useful or effective.
It is likely that several hundred thousand people will die from the infection in the coming months. Yet similar numbers die each year from seasonal flu, not to mention tuberculosis and other infectious diseases. The attention and resources drawn to tackling coronavirus, and its impact on health workers, will lead to neglect of patients with other conditions.
Isolation, treatment and other emergency health measures against Covid-19 may help defer fatalities among those most at risk, notably the elderly and those with fragile immune systems. Yet many will soon succumb to other conditions, including different respiratory viruses.
Draconian quarantine measures in China appear to have slowed the spread. Yet even if such measures could be replicated elsewhere, overreaction poses dangerous risks, including depressed economic growth costing people their jobs.
Despite shortcomings, progress has been made since previous pandemics with faster disclosure of new infections, swifter sharing of their characteristics with international researchers, and advances in the development of potential vaccines.
Longer term, the biggest question is whether the world will give greater priority to investing in the prevention of future pandemics. That requires more focus on links between health and the environment including “one health” measures to limit the spread of animal infection to humans. Examples include tougher controls on their intensifying interactions through climate change, deforestation and “wet markets” where live animals are sold for slaughter.
The situation also demands far greater efforts to strengthen health systems, boosting their resilience to future infections, whatever and wherever they may be.
Recommended links
- Official guidance (WHO)
- Latest news (FT)
- Data and maps (FT)
Ask the expert
David Heymann, former assistant director-general at the WHO who oversaw its response to Sars, will answer your questions on coronavirus before our next issue. Email health@ft.com or tweet us @fthealth. More details to follow on our Twitter feed.
Three questions
Prof Sir Michael Marmot, director of the UK’s UCL Institute of Health Equity and author of Healthy Equity in England: The Marmot Review 10 Years On
- What was your most unexpected finding?
I really did not expect life expectancy to have stalled. It took us all by surprise. If you were going to take the kind of decisions made by governments since 2010, it seemed likely that inequalities would increase but I did not anticipate life expectancy would fall for the bottom 10 per cent of the most deprived women living outside London. This is really a very troubling picture. Child poverty rose, there was the closing of centres for young people, the gig economy, insecurity and stress at work. - Can you prove inequalities are the reason for declining health outcomes?
In the 2010 review we identified the causes of health inequalities [according to] . . . more than 80 experts. If we know the causes and the adverse trends, it’s a reasonable supposition to say inequalities in some part have been responsible for the slowdown [in outcomes]. In 2010, 42 per cent of GDP went to public expenditure, by 2018 it was 35 per cent. The global financial crisis and the policies put in place after it were drivers. Brexit is a symptom not a cause. - How can the trend be reversed?
We call on the prime minister to set a national strategy for a reduction in health inequalities. We want leadership from the top. If he is serious about levelling up, investment in infrastructure by itself won’t do it. We need to increase spending on public health prevention to 7 per cent of the NHS budget; give every child the best start in life; create fair employment and good work; ensure a healthy standard of living for all; create and develop healthy and sustainable places and communities; and strengthen the role and impact of ill-health prevention.
FT: Gains in UK life expectancy stall after decade of austerity
Focus on . . . the cost of obesity
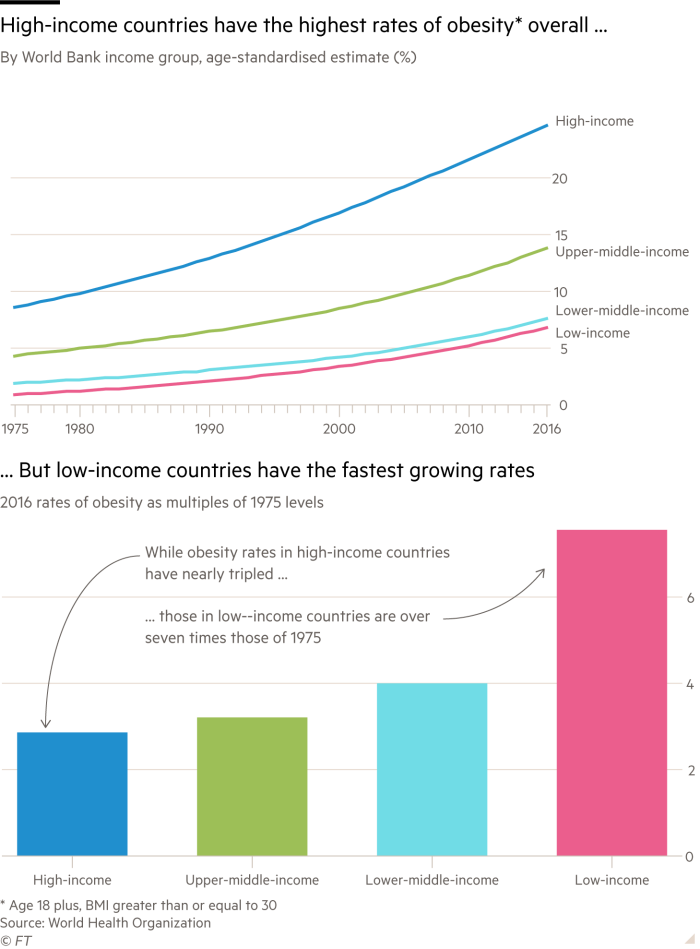
World Obesity Day is a time to highlight the increasing burden on poorer countries, as shown by the WHO data above. A World Bank report said more than 70 per cent of the world's 2bn overweight and obese individuals live in low- or middle-income countries. The knock-on effects of increased disability, early deaths, healthcare costs and lower productivity could cost developing countries more than $7tn in the next 15 years. The scientific community pledged to end the stigma of obesity. (WHO, World Bank, Nature).
News round-up
Health spending Even before coronavirus became a global threat, WHO Chief Tedros Adhanom Ghebreyesus urged world leaders in Davos to increase their health spending by 1 per cent of GDP. This would boost primary care systems by more than $200bn a year and save more than 60m lives. The WHO published a digital version of its essential medicines list to help countries spend smarter. It also outlined its health priorities for the next decade. (Health Policy Watch, WHO)
Struggle against superbugs Pharma companies have made some progress on antimicrobial resistance, but not enough to make a real difference, according to an annual benchmark. Low-income countries are particularly at risk. An industry report said governments must provide new incentives for later stage R&D. On the positive side, artificial intelligence has been used to discover a new antibiotic for previously untreatable diseases. (Access to Medicine Foundation, Guardian, AMR Industry Alliance, FT)
Disease R&D The annual G-Finder report showed record funding for research into HIV/aids, malaria, TB and other “neglected” diseases, with the EU now the third biggest funder after the US and UK. No donor country yet meets WHO-recommended levels of investment. (Policy Cures Research)
Gates and Gavi Bill and Melinda Gates look back at 20 years of their foundation and the $53.8bn it has spent, 29 per cent of it on global health. It helped set up The Global Fund to Fight Aids, Tuberculosis and Malaria; and Gavi, the Vaccine Alliance, which has helped vaccinate more than 760m children and lower market costs. (Gates blog)
Malaria milestones Malawi, Kenya and Ghana introduced the first — and only — vaccine for malaria. It is only 40 per cent effective but experts hope it can help as progress against the disease stalls. The operation has attracted some criticism however over ethical standards. Kigali in Rwanda will host the world's first summit on malaria and neglected diseases in June. (Stat, BMJ, End Malaria)
Fighting fake news The WHO turned to TikTok, the viral video app, to help its fight against health misinformation. Facebook said it wanted to build trust with the public sector following the rise of vaccine hesitancy. Coronavirus has become a ‘Petri dish’ for conspiracy theories, which are spreading almost as fast as the virus itself. New research shows how damaging false information can be. (The Verge, Devex, Wired, Vanity Fair, University of East Anglia)
Mind the aid gap Humanitarian emergencies have been increasing over the past few years but the shortfall in aid funds is widening. Less than half the amount needed for health emergencies has materialised, the WHO said. (The Lancet)
Britain after Brexit The UK may now be outside the EU but can still play a pivotal role in global health, for example by making markets work better for the poor. Speculation still surrounds the long-term future of The Department for International Development. Our science editor considers whether Brexit will irreparably damage the UK’s science base. (Center for Global Development, Guardian, FT video).
Tackling illegal drugs Dame Carol Black published her government-commissioned report on the supply and demand of illegal drugs in the UK. She estimated the illicit market was worth £9.4bn a year but the overall cost to society was twice as much. (UK government)
Drone Academy Unicef and the Malawi government opened the first African Drone and Data Academy, where students can learn to build and pilot drones. Africa's first “humanitarian corridor” was launched in the country in 2017 to test the transport òf supplies such as medicines and blood samples. Watch our video on how drones and other innovations are transforming access to healthcare.
Data privacy Google trumpeted its use of AI to detect breast cancer, but some critics cast doubt on whether the company can be trusted with our healthcare data. The head of parent company Alphabet wrote for the FT on the need for regulation: “Companies such as ours cannot just build promising new technology and let market forces decide how it will be used.” An FT investigation revealed how top health websites were sharing sensitive data with advertisers. (FT)
Smoke signals The transatlantic divide over vaping continued apace as the US cracked down on flavoured products while British authorities promoted its role in weaning people off cigarettes. One researcher warned of “hot stuff bias” where topics with a lot of media attention can attract a disproportionate amount of bad science. (Guardian, NYT, NHS, The Conversation)
Road safety Road traffic incidents kill 1.35m people a year — 93 per cent of which are in low- and middle-income countries — and are the leading cause of death for children and young adults. A global summit in Stockholm committed ministers to accelerate efforts to halve road traffic deaths and injuries by 2030. (UN News, Jakarta Post)
Burden of cancer Cancer will hit poorer countries disproportionately harder over the next two decades, according to the World Cancer Report. Current trends suggest a 60 per cent jump in cases with more than 80 per cent in low- and middle-income countries. More than 91 per cent of richer income countries provide comprehensive treatment services, compared with less than 15 per cent in their poorer counterparts.
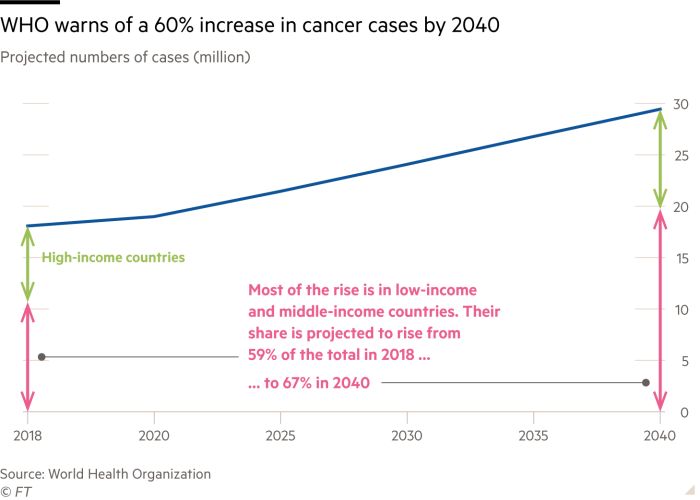
Other reports released ahead of World Cancer Day showed outlooks for cervical cancer, public perceptions of the disease, and a UK study of the “ripple effect” of cancer costs on society. (WHO, The Lancet, NCD Alliance, Demos)
Public health The annual festival this week of The International Society for Neglected Tropical Diseases was another reminder, from comics to online games, that communicating complex issues can be done in a fun and engaging style.

Best from the journals
Deadly air pollution A study using new methodology said air pollution now rivalled smoking as a cause of early death. It is associated with an extra 8.8m premature deaths in 2015, representing a reduction in life expectancy of almost three years. (Cardiovascular Research)
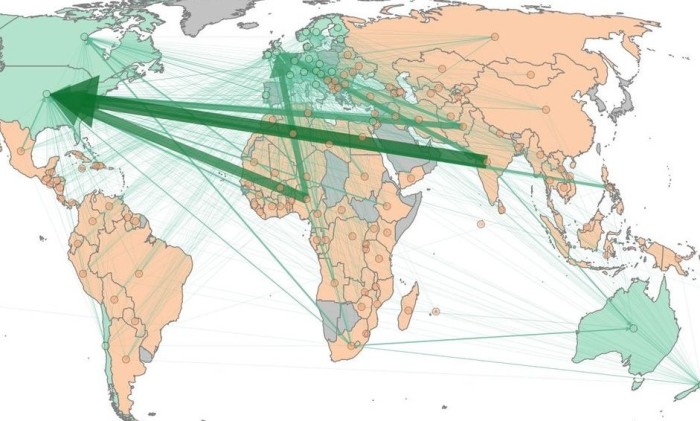
Brain drain The migration of doctors to richer nations means more early deaths and an $16bn annual economic loss for their home countries. Arrows on graphic show direction of migration, while thickness shows cost to source country. (BMJ)
Child health Children around the world are being let down by their governments, according to a new index which ranks countries' performance on everything from health and education to protection from exploitative marketing and failure to tackle climate change. Kids in Norway fare the best and those in Central African Republic the worst. (WHO/Unicef/Lancet)
Drug prices A special issue of The Journal of the American Medical Association includes studies on how much R&D investment is needed to bring a drug to market and how the profits of Big Pharma compare with other large public companies. (JAMA)
Health inequalities Prof Marmot — see Three Questions above — is not alone in linking social deprivation with ill health. A Lancet study and editorial said it was essential to evaluate welfare policies from a public health perspective to avoid prolonging or worsening inequalities. The Royal College of Paediatrics and Child Health found health outcomes for UK children from disadvanted backgrounds were up to four times worse than for their better-off counterparts. (The Lancet, RCPCH)
Pick of the pods
Urban health How do you build a healthy city? FT correspondents discuss initiatives in six cities, from tackling loneliness in Copenhagen to promoting healthier eating in Tokyo.
Pandemic preparedness Discussion on trends in global investment for health security and the call for the World Bank to set up a Pandemic Preparedness Challenge. (CSIS Take as Directed, 27m)
Neglected tropical diseases Discussing the efforts by governments and NGOs to eliminate the diseases that affect 1.7bn people (UN Global Dispatches, 30m)
Drug prices How can we improve the function of the market for medicines without damaging access for the poor? (BMJ Talk Medicine, 26m)
Medicine made for you Three-part series on the personalisation of healthcare. (Anthill podcast/The Conversation)
The month ahead
March 5, 10, 17, 24: New episodes of FT How to Build a Healthy City podcast
March 10: FT report on Combating Diabetes
March 24: World TB Day
April 1: Next edition of FT Health
End notes
Health at Work Join our quest to find Britain’s healthiest workplaces
Digital health Submit your ideas to the FT/Lancet Commission on how AI and digital health developments can benefit the world’s poorest.
FT resources You can find all FT in-depth health reports at FT Health Centre.
Contact Email us via health@ft.com, like us on Facebook and follow us on Twitter @fthealth and LinkedIn.
FT Health by email Register here to get FT Health in your inbox on the first Wednesday of each month.
Final thought
Scotland is set to be the first country in the world to make women’s sanitary products free. Should others follow?
Comments